- Home
- About
About
About Us
Advancing Mpox research for healthier pregnancy outcomes
Mission Statement
To advance research, surveillance, and clinical interventions focused on Mpox in pregnant women, ensuring evidence-based strategies for prevention, early detection, and treatment. Through scientific innovation, collaboration, and advocacy, we strive to protect maternal and neonatal health from the impacts of Mpox.
Vision Statement
A world where Mpox in pregnancy is well understood, effectively managed, and no longer a threat to maternal and neonatal health—where every pregnant woman has access to timely diagnosis, optimal care, and interventions, ensuring the best outcomes for both mother and child.
Transforming lives
with unwaivering commitment

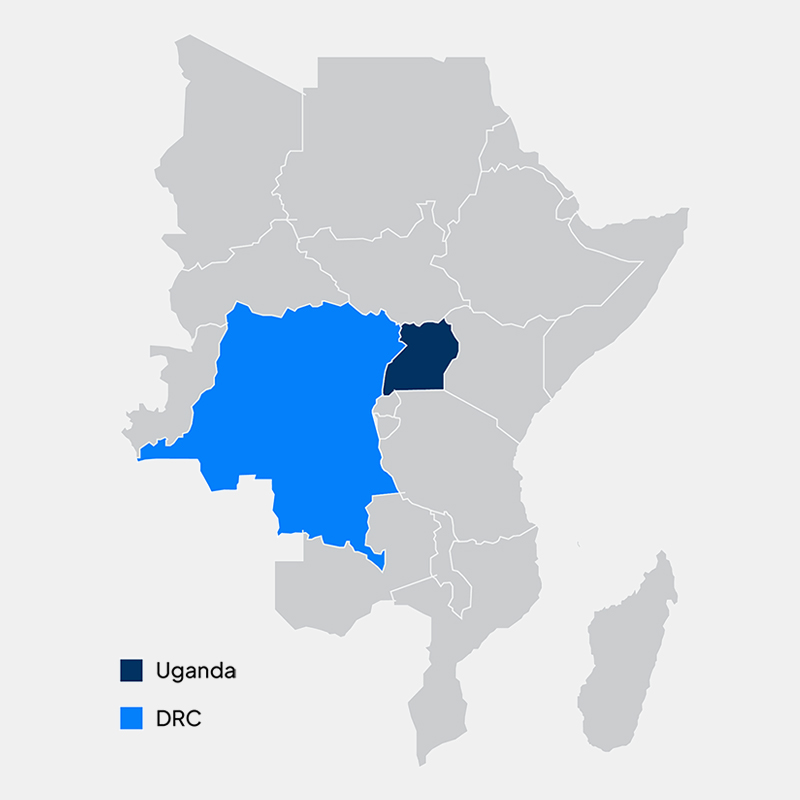
Where we work
Africa is home, and our hearts long to see every pregnant mother thrive with no risk of Mpox.

Mpox and Pregnancy: Understanding the potential risks and implications
During pregnancy, a woman’s immune system undergoes changes to support both mother and fetus. While essential for a healthy pregnancy, this immune modulation also creates vulnerabilities—particularly to infections like Mpox (MPXV).
To prevent fetal rejection, certain immune responses are suppressed, making it harder to fight infections. As a result, Mpox can cause more severe and prolonged illness, with higher fevers, extensive skin lesions, and increased fatigue. In some cases, slower viral clearance raises the risk of complications, potentially requiring hospitalization, intensive monitoring, or advanced medical care, posing a serious threat to both mother and baby.
Mpox (MPXV) infection during pregnancy poses a serious risk to both the mother and fetus, increasing the likelihood of complications. One major concern is preterm labor, as infections can trigger early contractions, leading to premature birth. Preterm infants often face developmental delays, lung and brain complications, and weakened immunity.
In more severe cases, miscarriage risk is heightened, particularly in the first trimester, when pregnancy is most vulnerable. If the infection worsens, it may also lead to stillbirth, especially if MPXV affects placental function or fetal development. These risks highlight the importance of early detection, close monitoring, and timely medical intervention to improve pregnancy outcomes.
Vertical transmission occurs when a virus is passed from mother to fetus during pregnancy, and Mpox (MPXV) is no exception. While research on MPXV’s transmission in pregnancy is still limited, it remains a serious concern. If the virus crosses the placenta, it can cause congenital Mpox, leading to symptoms at birth or soon after, such as fever, rashes, and respiratory distress.
The severity of vertical transmission depends on the timing of infection and the mother's health. In some cases, it may lead to developmental issues, birth defects, or long-term complications. More severe instances can result in neonatal death. These risks highlight the urgent need for preventing and managing Mpox during pregnancy to safeguard both maternal and infant health.
Severe Mpox (MPXV) infection during pregnancy can pose a life-threatening risk if not properly managed. The virus may cause high fever, widespread rashes, and respiratory distress, potentially overwhelming the body's ability to recover. Pregnancy further increases vulnerability, as the immune system is naturally suppressed to protect the fetus, making it harder to fight infections effectively.
In extreme cases, untreated or poorly managed Mpox can lead to sepsis, organ failure, or respiratory collapse, significantly increasing the risk of maternal death. Timely medical intervention, intensive monitoring, and supportive care are crucial in preventing severe complications and improving outcomes for both mother and baby.
Mpox (MPXV) infection during pregnancy can disrupt fetal growth, leading to serious complications. The virus may cause intrauterine growth restriction (IUGR), malformations, or organ damage if it crosses the placenta, increasing the risk of physical or neurological abnormalities. Additionally, placental insufficiency may occur, reducing oxygen and nutrient flow to the fetus, further impairing development.
In some cases, Mpox exposure in the womb may result in long-term developmental delays or congenital abnormalities. The severity of these effects depends on the timing of infection and the overall health of both mother and fetus, emphasizing the need for early detection and proper management to protect fetal development.
Our Strategic Objectives
Assess the Impact of Mpox on Pregnancy
Investigate how the Mpox virus (MPXV) affects pregnant women, including their susceptibility to infection, the severity of illness, and potential complications during pregnancy. Special attention will be given to understanding the likelihood of vertical transmission to the foetus and the possible long-term effects on maternal and infant health.
Characterize Clinical Features and Risks
Collect and analyze clinical data on mpox-infected pregnant women to identify common symptoms, disease progression patterns, and potential risk factors that contribute to severe outcomes. This information will help healthcare providers recognize cases early and implement appropriate medical interventions to reduce complications.
Map the Geographical Spread of Mpox in Pregnant Women
Conduct both passive and active surveillance to track the spread of mpox among pregnant populations in South Kivu and possibly neighboring regions. Passive surveillance will involve analyzing data from health facilities to identify reported cases, while active surveillance will engage communities to uncover unreported cases. This mapping will provide valuable insights into spatial risk factors, social determinants, and environmental contributors to mpox transmission in these regions.
Evaluate Pregnancy Outcomes Associated with Mpox
Examine the direct and indirect consequences of MPXV infection on pregnancy outcomes, including risks of miscarriage, stillbirth, preterm birth, and other maternal or neonatal complications. The study will also explore whether certain maternal health conditions or external factors increase the likelihood of adverse outcomes in mpox-infected pregnancies.
Investigate Immune and Pathological Responses
Assess the immune response of pregnant women to MPXV infection to determine how their immune systems react to the virus and whether pregnancy alters the severity of infection. Additionally, placental samples will be analyzed to identify any pathological changes caused by the virus, helping to determine the mechanisms behind vertical transmission and pregnancy-related complications.
Examine the Safety and Effectiveness of Mpox Interventions
Evaluate the impact of the MVA-BN vaccine and tecovirimat antiviral treatment on pregnant women by monitoring their safety, effectiveness, and potential adverse effects. A comprehensive registry will be developed to document pregnancy-related complications linked to these interventions, helping policymakers and healthcare providers make informed decisions about their use in pregnant populations.
Enhance Public Health Preparedness and Response
Generate critical data to improve screening, diagnosis, and management strategies for Mpox in pregnancy. The findings will contribute to refining public health policies, guiding treatment protocols, and shaping epidemic control measures to mitigate the impact of Mpox on pregnant women and their communities.
Raise Awareness and Promote Preventive Measures
Develop targeted educational campaigns to inform communities about the risks of mpox during pregnancy, preventive strategies, and the importance of seeking medical care early. By increasing awareness and engagement, the project aims to encourage better health-seeking behaviors, improve case reporting, and strengthen community-level prevention efforts.